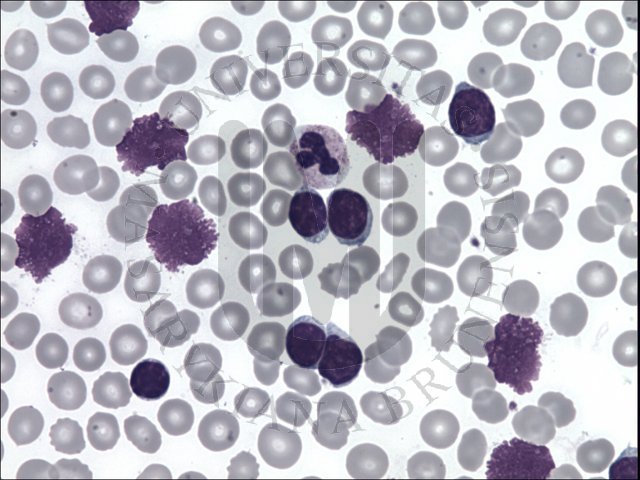
ARID1A loss correlates with high-grade endometrial carcinomas
BAF250a (ARID1A) loss is a frequent event in high-grade endometrial cancers. It has been proposed that ARID1A is a driver gene, with ARID1A mutations occurring secondary to deregulated mismatch repair mechanism in gastric cancers, representing an alternative oncogenic pathway to p53 alteration. The prognostic significance of ARID1A loss is controversial. In this study, we investigated the frequency of BAF250a immunohistochemical loss in a cohort of high-grade endometrial cancers (n=190) and correlated it with mismatch repair (hMLH1, hMSH2, hMSH6, and hPMS2) and p53 protein expression. The 190 cases consisted of 82 high-grade endometrioid, 88 serous, 10 clear cell, and 10 mixed (carcinosarcomas and mixed histology). There was BAF250a loss in 55/190 (29%) cancers, most commonly in high-grade endometrioid carcinomas (46 vs 9% in serous carcinomas, P<0.0001). Loss of any mismatch repair proteins was observed in 63/190 (33%) cancers, most commonly in high-grade endometrioid carcinomas (57 vs 10% in serous carcinomas, P<0.0001). Aberrant p53 expression was found in 86/190 (45%) cancers, more commonly in serous carcinomas (77 vs 18% in high-grade endometrioid carcinomas, P<0.0001). BAF250a loss was associated with mismatch repair loss (P<0.0001) and normal p53 expression (P<0.0001). These associations were maintained in the subset analysis within the high-grade endometrioid (P=0.026 and P=0.0083, respectively) and serous carcinoma cases (P=0.0031 and P<0.0001, respectively). Survival analysis revealed a superior progression-free survival (P=0.017) for patients with BAF250a loss within the entire cohort but not within the high-grade endometrioid and serous subtypes. Additionally, data from The Cancer Genome Atlas were extracted to correlate mutations in ARID1A, TP53, and MMR genes; we found that ARID1A mutations were negatively associated with TP53 mutations but were unrelated to mismatch repair gene mutations. In conclusion, BAF250a loss is more common in high-grade endometrioid carcinomas than in other high-grade endometrial cancers and is associated with mismatch repair deficiency and normal p53 expression.




 با سلام...
با سلام...